Hypertension, the medical term for a diagnosis of high blood pressure, is a major risk factor for stroke, heart attacks, kidney failure, heart failure, blindness, amongst other significant issues. Left ignored, hypertension can cause irreparable damage. As a certified hypertension specialist and director of the Toronto Hypertension Clinic, I have educated and treated thousands of patients in achieving effective blood pressure control.
The following are my answers to the Top 10 Questions I receive from patients in clinic:
1. What causes high blood pressure?
High blood pressure in most individuals occurs because of a combination of factors as opposed to one single cause. Major contributing factors include increasing age, obesity, lack of exercise, excess salt consumption, ethnicity, strong family history of hypertension, excess alcohol, and poor sleep. A smaller subset of individuals (5-10%) have 'secondary hypertension', wherein an additional medical condition is causing blood pressure to be elevated. Such conditions include chronic kidney disease, obstructive sleep apnea, excess aldosterone hormone (primary aldosteronism), excess cortisol hormone (Cushing's syndrome), kidney artery occlusion (renovascular hypertension), overactive and underactive thyroid conditions, and more. Testing for these conditions is guided by clinical suspicion and treatment resistance.
2. How do systolic and diastolic blood pressure change with age?
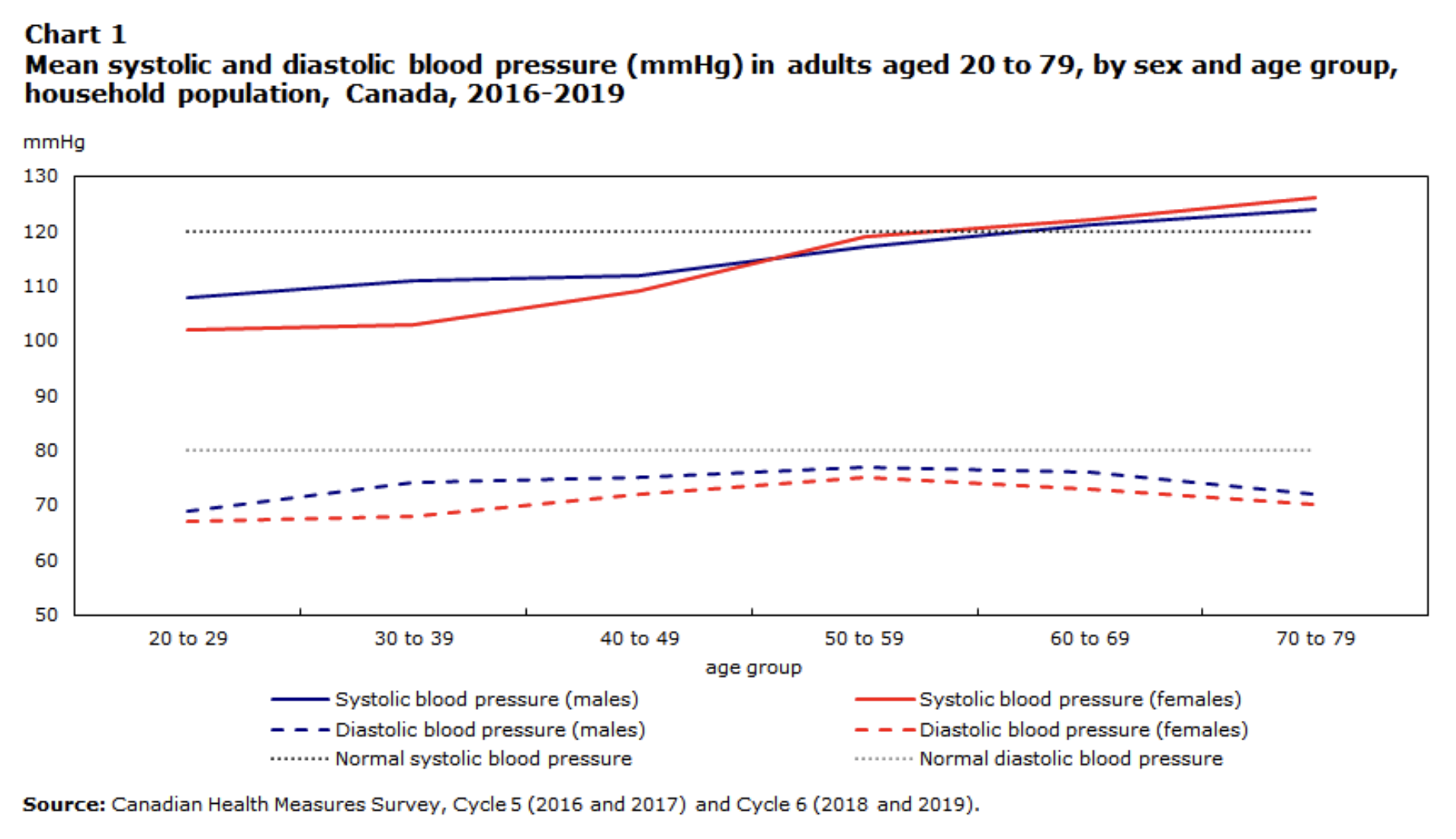
For a blood pressure of 120/80mmHg, the systolic blood pressure (120) represents the maximum pressure an artery wall faces when blood is passing through. The diastolic blood pressure (80) is the pressure in the artery wall during relaxation, in-between heart beats. Controlling both numbers is important to prevent cumulative damage to the blood vessels over time. As depicted in the graph below, earlier in life women tend to have a lower systolic blood pressure than men, before rising faster on average from 45-55 years old. For an individual who is middle-aged, it is common to have a 'diastolic-predominant' form of hypertension. The diastolic blood pressure tends to reach a maximum around the age of 55 and gradually lowers in later life. By contrast, the systolic blood pressure continues to rise with age due to increased arterial stiffness, with arteries that are more calcified and less elastic. It is therefore common for an individual in their 80s or 90s to have a large difference between the systolic and diastolic blood pressure numbers.
3. What foods or diet best lowers blood pressure?
Effective dietary changes should be a part of any hypertension treatment plan. The DASH diet (Dietary Approach to Stopping Hypertension) is a Mediterranean-type diet that has the best evidence for lowering blood pressure. It contains less-processed foods such as fruits and vegetables, low-fat dairy products, lean protein (fish and poultry instead of red meats), beans, nuts, and seeds. Sodium intake should be restricted to a maximum of 2000mg per day, with additional avoidance of high fat, highly-processed, and sugary foods.
4. What effect do alcohol, smoking, and caffeine have on blood pressure?
Consuming a small amount of alcohol (e.g. 1-2 drinks per week) is unlikely to have a major impact on blood pressure, but when alcohol is consumed in higher amounts on a regular basis, cutting down can modestly improve blood pressure control, in addition to several other health benefits. Smoking typically causes a transient increase in blood pressure with cumulative effect if smoking consistently over the course of a day. Smoking is damaging to blood vessel walls, and has major long-term health consequences from cardiovascular, respiratory and cancer perspectives. Caffeine consumption in small to moderate amounts, such as with a daily coffee or tea, is safe for those with high blood pressure.
5. Is it safe to exercise with high blood pressure?
Yes, exercise is safe and net beneficial for those with hypertension. Regular, moderately-intensity aerobic exercise has been shown to help lower blood pressure over time, amongst multiple other health benefits. It is a normal physiological response for blood pressure, similar to heart rate, to temporarily rise during exercise. This is not considered dangerous, and it is not necessary to monitor blood pressure during routine exercise. If you are experiencing dizziness with low blood pressure from your medication, consider temporary avoidance or modification of exercise activity to prevent loss of consciousness and/or injury.
6. What are the common symptoms of high blood pressure?
Symptoms are not a reliable indicator of high blood pressure and most individuals with hypertension have no symptoms at all. A small subset of individuals may experience a band-like headache or in rare cases a nosebleed with blood-pressure spikes. Symptoms of low blood pressure often involve dizziness, fatigue, and light-headedness.
7. When should I go to the emergency department with high blood pressure?
A hypertensive emergency is a systolic blood pressure that is greater than 180mmHg and/or diastolic blood pressure greater than 120mmHg with symptoms and signs that suggest acute organ damage: stroke or intracranial hemorrhage (brain bleed), a heart attack, aortic dissection, or pre-eclampsia / eclampsia. In all other situations (hypertensive urgency) there is no indication for rapid blood pressure lowering, and medication should be titrated gradually over weeks to months to allow time for the body to adapt and to avoid potential harm.
Many individuals may notice a blood pressure 'spike' in the context of acute physical or psychological stress, with sympathetic nervous system activation and subsequent release of fight or flight hormones. Common situations of blood pressure spikes include physical injuries or pain flares, acute sleep deprivation, anxiety, panic attacks, amongst others. It is therefore important to recognize and address any alternate factors causing acute blood pressure elevation, allow time for stress to settle and further monitoring, and to treat the overall blood pressure average as opposed to outlier readings.
8. How often should I check my blood pressure?
When making a hypertension diagnosis, starting or switching medications, or altering a medication dose, blood pressure should be measured more frequently: twice a day, once first thing in the morning and once just before bed. Monitoring frequency can be reduced during periods of blood pressure stability. To accurately measure your blood pressure, you should do so after being seated and relaxed for 5 minutes and use the same arm each time. Your arm and back should be firmly supported with your feet firmly planted on the floor. Take 2 readings separated by a couple minutes on each occasion. To avoid false elevations, I encourage my patients to check their blood pressure only they are feeling calm, relaxed, and pain free. It is not necessary to monitor blood pressure repeatedly throughout the day or in the middle of the night. Treatment decisions regarding medication should be based on blood pressure averages as opposed to single readings.
9. When is blood pressure medication recommended and what is my target blood pressure?
As per Hypertension Canada, for most individuals blood pressure medication is recommended when blood pressure is consistently greater than 140/90mmHg. For those with diabetes, medication is recommended for blood pressure greater than 130/80mmHg. For some individuals at high risk of stroke, heart attack, or kidney failure, a more aggressive target of systolic blood pressure less than 120mmHg may be recommended. For those who are mildly above target range, a short period of lifestyle intervention alone may be reasonable, with medication to be started if this is not successful.
10. Can I stop my blood pressure medication once my blood pressure is controlled, or will I need to take it indefinitely?
Once blood pressure is under control with medication, it should be continued regularly at that dose indefinitely. As blood pressure naturally increases with age, most individuals who are started on blood pressure medication will need to continue it indefinitely, especially in the absence of major lifestyle changes such as: weight loss, significant dietary changes, exercise, etc. Discuss with your physician if you are considering stopping or reducing your blood pressure medication.
For more information on high blood pressure, we recommend reviewing Hypertension Canada's educational resources: https://hypertension.ca/resources/public/
